UCSF Center of Excellence
What We Believe In
We believe in women and are working to transform their health and lives.
We believe women deserve healthcare and health policy that is based upon rigorous research inclusive of sex and gender variables, designed with community, and provided compassionately by clinicians who respect individual values and choices.
Healthcare
Providing women-focused care across the lifespan guided by patient choice.
Research
Pioneering discovery and innovation in women’s health through sex and gender inquiry.
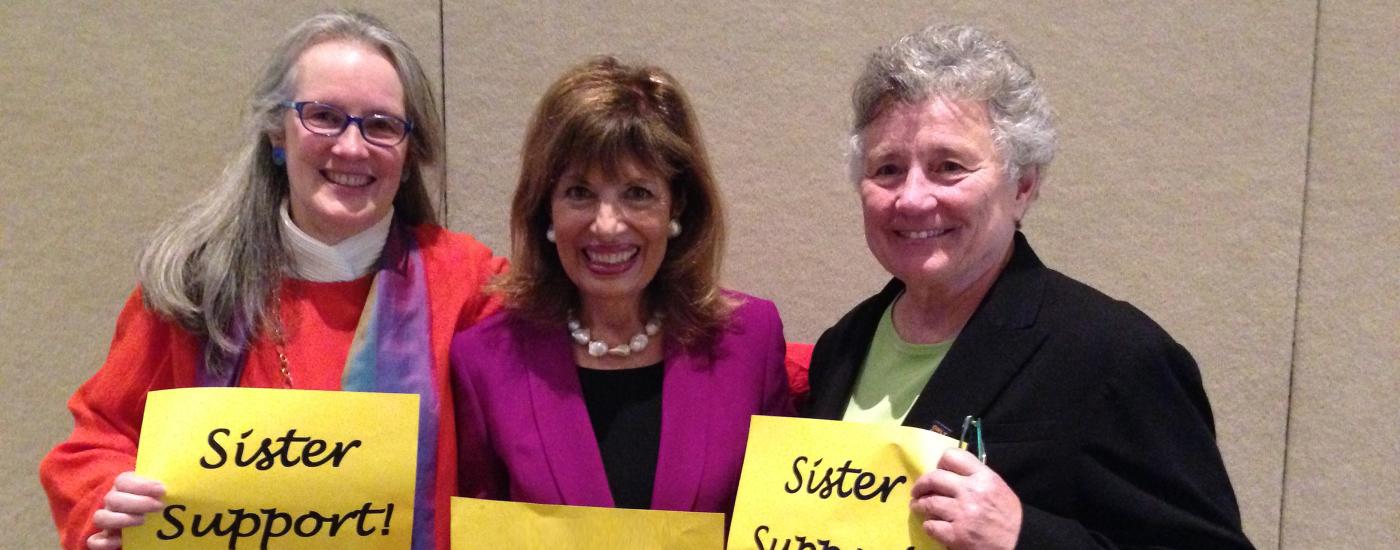
Leadership
Recognizing and fostering women leaders in health and science.
Community
Partnering with communities to promote women’s health and well being.
Education
Educating the next generation of women’s health providers, scientists and policy makers.
Director’s Spotlight
Kai Kennedy, DPT
Made to Scale: Can We Grow More Equitable Health Care?
What keeps you up at night?
For Kai Kennedy, DPT, it’s health equity – a complex mission that’s guided a lifelong journey from Virginia to West Africa, the Caribbean to Europe and now the Bay Area. But she didn’t get here alone.
“My teachers are all around me. Your teachers are all around you, too,” she told the crowd at UC San Francisco’s Mission Bay campus on April 12. Kennedy presented her inspiring story as part of UCSF’s annual Last Lecture program, a student-initiated series where a nominated faculty member shares the professional, personal, spiritual and cultural experiences that have shaped them.

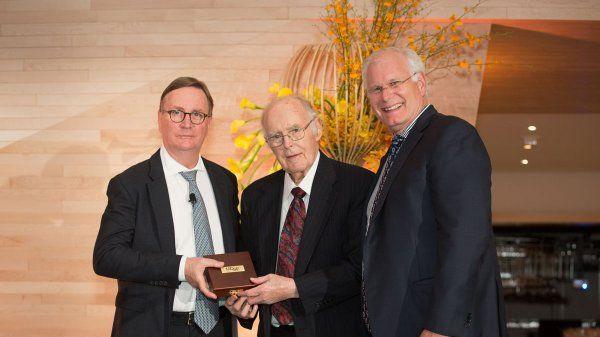
Honoring Dr. Nancy Milliken, MD
With deep gratitude, we bid a fond farewell to our Founding Director, Dr. Nancy Milliken, as she retires after almost 40 years at UCSF. Dr. Milliken dedicated her career to eliminating health disparities for women. Help us honor this incredible legacy by supporting our efforts to endow a professorship for women’s health leadership in Dr. Milliken’s name. These funds will ensure that improving women's lives remains a priority at UCSF for decades to come.