UCSF Center of Excellence
What We Believe In
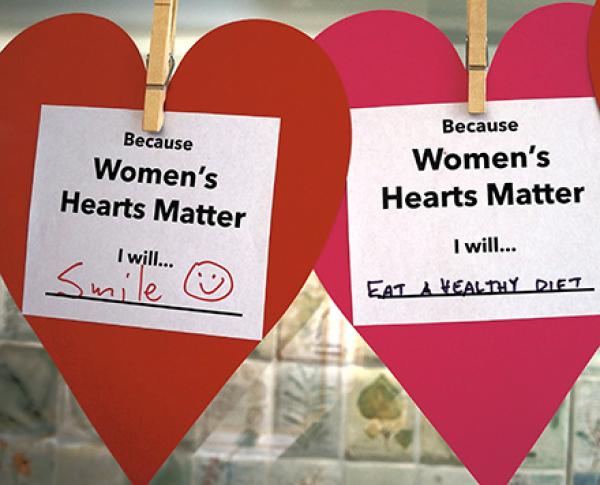
We believe in women and are working to transform their health and lives.
We believe women deserve healthcare and health policy that is based upon rigorous research inclusive of sex and gender variables, designed with community, and provided compassionately by clinicians who respect individual values and choices.
Director’s Spotlight
Black Womxn’s Health & Livelihood Initiative Celebrates 5 Years!
Surrounded by community members, partners, patients, allies, and friends, the Black Womxn’s Health and Livelihood Initiative (BWHLI) recently gathered to celebrate the past five years of collaboration, connectivity, and serving our community. We gathered to recognize and honor that we have worked to provide quality health care, create innovative programs, strategize and implement necessary systems change, and care for and nurture our beautiful Black community. We celebrated the impact we’ve made addressing health and health care disparities for Black womxn and our gender expansive communities.

Healthcare
Providing women-focused care across the lifespan guided by patient choice.
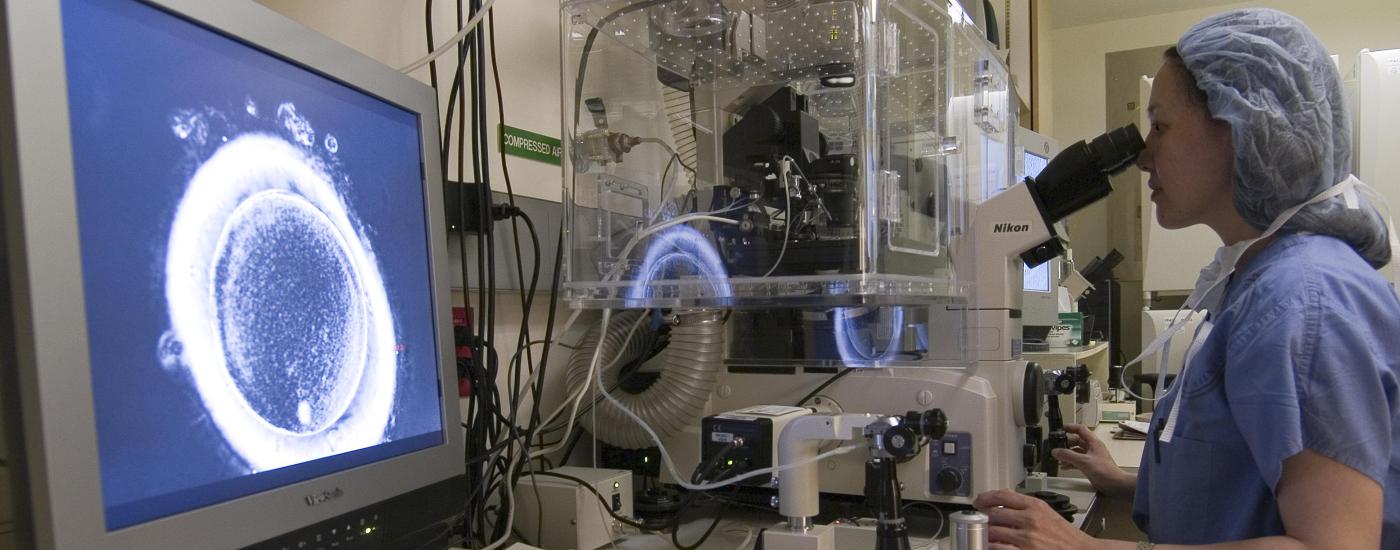
Research
Pioneering discovery and innovation in women’s health through sex and gender inquiry.
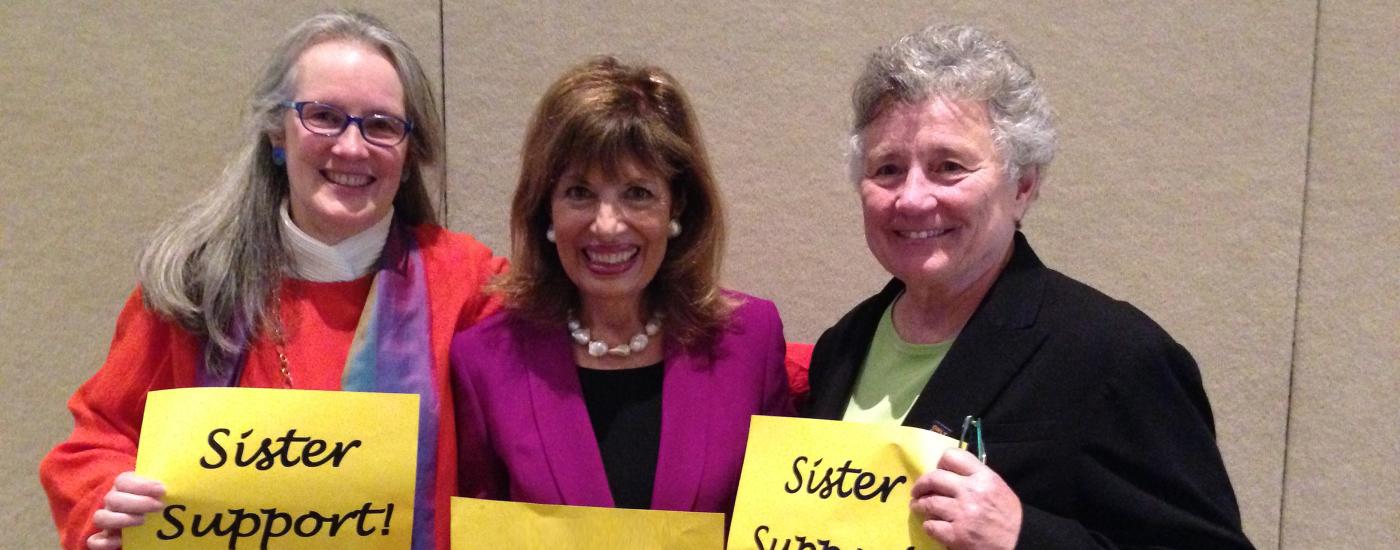
Leadership
Recognizing and fostering women leaders in health and science.
Community
Partnering with communities to promote women’s health and well being.
Education
Educating the next generation of women’s health providers, scientists and policy makers.